The British government is being called to investigate the astonishing amount of BAME workers who are dying due to Covid-19.
NHS England has called upon health trusts to assess (BAME) workers who are “at potentially greater risk” from coronavirus. One in five of the 1.3 million NHS staff are from BAME backgrounds. The Guardian uncovered that out of 53 NHS staff who have died 68% were BAME. 22 nurses, two porters, a radiology support worker, a patient discharge planner and a hospital bus driver. There are more minority ethnic people working in the NHS 20%, rising to 44% for medical staff. As a result, the rate of mortality is seriously uneven.
Data from the Intensive Care National Audit and Research Centre suggests 34.5% of Covid-19 patients who are critically ill are from BAME backgrounds. Despite only 10.8% of the population is black or Asian, according to the 2011 census.
The first 10 doctors in the UK who died from coronavirus were all BAME. Dr Adil El Tayar was the first BAME worker to die from Covid-19. He was a 63-year-old Sudanese heart surgeon. He was volunteering in an A&E department in the Midlands and died on 25 March at West Middlesex University Hospital in Isleworth in West London.
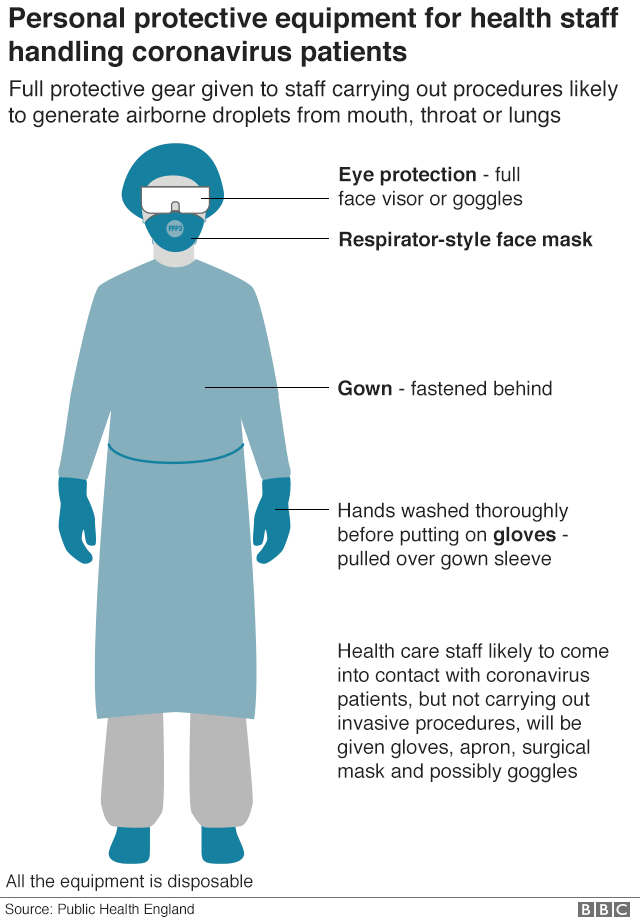
On Wednesday 8th April, Bangladeshi doctor, Abdul Mabud Chowdhury, 53, died from Coronavirus. yet he had no underlying conditions. Before he died he wrote a letter to the government asking for adequate provisions of PPE to protect workers.
His son Intisar Chowdhury, 18, wrote a later to the government questioning why his father’s letter to Boris Johnson was ignored.

Intisar Chowdhury said: “When he was unwell he wrote an open letter to the prime minister appealing for more PPE for NHS frontline workers, it was a request that was ignored, two weeks later he passed away and since then over 100 NHS and social care workers have passed away from contracting the virus,”.
The chronic lack of PPE has been a issue of hot debate and lives are being lost as a consequence of insufficient planning and prompt action.

https://twitter.com/inzyrashid/status/1252963871134035968
17 non-executive NHS directors of the Seacole Group, the largest network of BAME leaders within the service, have written to Mr Hancock, offering their services as an independent advisory group in hopes to address the deaths of BAME health and social workers.
Coronavirus continues to entrench the instiutional racism
There has been a long-held belief that institutions are nourished by racism and Covid-19 deaths have only reinforced and further evidenced this. The death rates of workers and those admitted only reaffirm this.
According to the Cabinet Office, (2019), black minority ethnic people are more likely to be key workers and/or work in positions where the threat of exposure is greater. Some of these positions include cleaners, public transport (including taxis), shops, and NHS staff.
Black and minority ethnic people are 40% of doctors, 20% of nurses nationally (and 50% in London). Within the NHS Black and minority ethnic people make up 17% of the social care workforce, and 59% in London.
The government have proven themselves chronically inept when dealing with the coronavirus pandemic; failing to buy crucial protective equipment, in turns affecting BAME staff who are at a far higher risk of contracting Covid-19 as they are the majority of the NHS workforce.
Cultural Reasons as to why BAME workers are more at risk
It has been said that cultural reasons are a key component resulting in COVID-19 killing more BAME workers. Covid-19 has a higher prevalence on those with underlying health issues, in particular, those suffering from obesity, high blood pressure and diabetes all more common amongst the BAME population. Further more Vitamin D deficiency is more common in people of an ethnic minority group.
In 2017 a study conducted highlighted that black adults were the most likely out of all ethnic groups to be overweight or obese. Obesity predisposes individuals to other issues such as diabetes and high blood pressure.
According to Diabetes UK , “Type 2 diabetes is up to six times more common in people of South Asian descent and up
to three times more common among people of African and African-Caribbean origin.”
Environmental factors play a part as to why underlying health issues are so prevalent in the BAME community. In black and minority ethnic groups on average poverty is twice as high. Poverty has a major correlation to obesity, access to overly processed and calorie-rich foods, resulting in poor nourishment puts the body at greater risk to health-related issues. Those with low socioeconomic status, healthier lifestyles may not always be a tangible reality, as money must be spent on other necessities such as rent. Black and minority ethnic families also tend to be larger on average, exacerbating stresses on the family and finances.
Ordinarily, a virus would not discriminate or stereotype on the basis of race or ethnicity. However, Covid 19 is massively affecting BAME NHS and front line workers. The government must do more to protect all those who protect and saves lives. Discrimination continues to seep through our institutions and rather than being a “great leveller”, the virus exposes the deep inequalities in the suffering of different communities. Focusing on genetics merely shifts blame; health inequality must be properly researched, measured and addressed. The government inquiry announced this month must publish data collected on ethnic minority deaths by Public Health England, to unravel uncomfortable truths, ensure wider understanding of the actual scale of threats BAME individuals and workers are facing and generate action.